

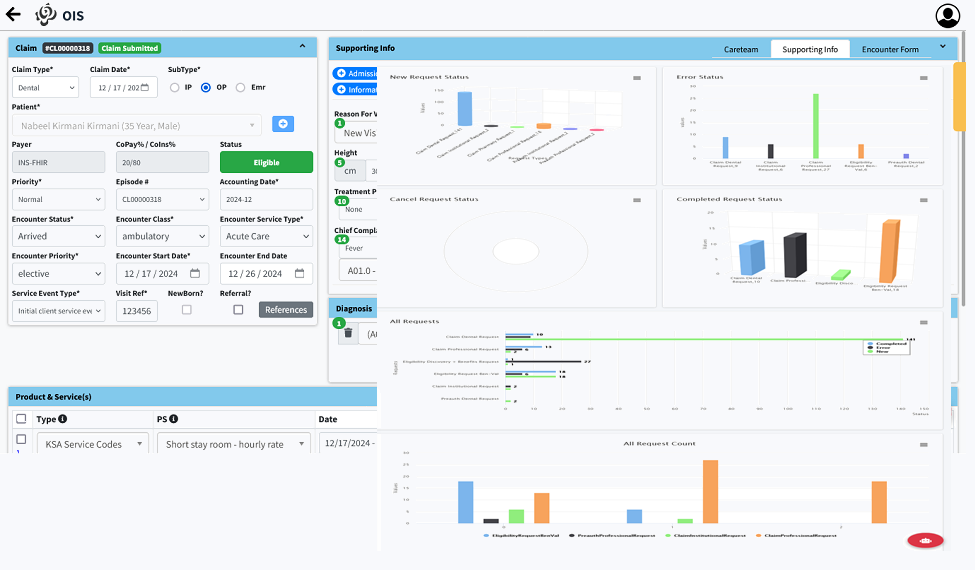
Our cutting-edge RCM application streamlines every aspect of the healthcare billing process, ensuring efficiency and compliance. Designed to support Eligibility Verification, Pre-Authorization, Claims Management, and Payment Reconciliation, the application caters to a wide range of healthcare needs, including In-Patient (IPD), Out-Patient (OPD), Pharmacy, Dental, and Vision Claims.
Powered by advanced AI assistance, the system simplifies workflows, reduces errors, and enhances decision-making for faster approvals and reimbursements. It is fully certified by NPHIES, guaranteeing compliance with regulatory standards in the healthcare industry.
Whether managing claims or reconciling payments, our RCM application ensures accuracy and reliability, helping you focus on delivering quality care while maximizing revenue. Experience a seamless billing process with AI-driven support, tailored for modern healthcare providers.
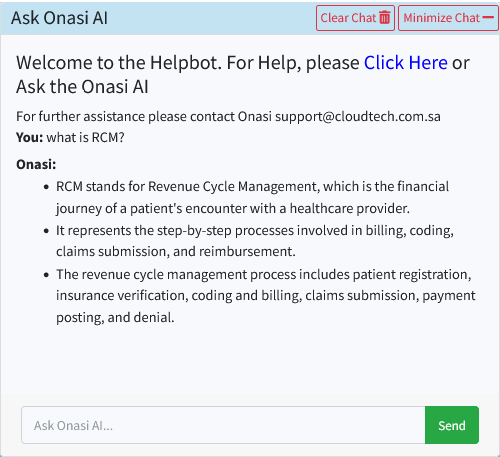
Onasi AI Claim Scrubber
The AI bot for Revenue Cycle Management (RCM) serves as an intelligent assistant, acting as an interactive user manual to guide users through various processes. It provides step-by-step instructions for complex tasks such as claim submissions, payment postings, and denial management, making it easy for users to navigate the system.
Additionally, the AI bot ensures compliance by verifying business rules and validation rules in real time. It identifies discrepancies, missing information, or non-compliance with payer-specific requirements before claims are submitted. This proactive approach reduces errors, improves claim acceptance rates, and enhances overall efficiency. By combining guidance and automated rule validation, the AI bot simplifies RCM workflows and empowers users to achieve accurate and efficient operations.

Why Choose Onasi RCM?
- HIS
- DHIS
- PHCS
- SAAS
- Cloud based
- On premises
ONASI simplifies decision making, streamlines operations, and ensures compliance with industry standards and best practices, ultimately saving time and effort to maximize value and returns.





